|
|
HEALTHY HAPPENINGS - July 2023
|
Can’t Get Off That Antidepressant?
by Ray Andrew, MD
|
 Before Carol started taking her antidepressant seventeen years ago, she often couldn’t drag herself out of bed to get to work in the morning. She stopped going to the gym. She couldn’t focus to get her work done. After work, she sat on the couch until it was time to climb into bed. Within a few weeks of starting her first antidepressant, she was back to herself again. Six months later, in accordance with national guidelines, her doctor suggested she stop taking the drug. Within a week, she became lethargic and developed a headache, achiness, insomnia, nightmares, nausea, lightheadedness, anxiety, irritability, vertigo, and strange sensations of being shocked in random parts of her body. Before Carol started taking her antidepressant seventeen years ago, she often couldn’t drag herself out of bed to get to work in the morning. She stopped going to the gym. She couldn’t focus to get her work done. After work, she sat on the couch until it was time to climb into bed. Within a few weeks of starting her first antidepressant, she was back to herself again. Six months later, in accordance with national guidelines, her doctor suggested she stop taking the drug. Within a week, she became lethargic and developed a headache, achiness, insomnia, nightmares, nausea, lightheadedness, anxiety, irritability, vertigo, and strange sensations of being shocked in random parts of her body.
Carol thought she had suddenly been smitten by some kind of a flu bug. But three weeks passed and her case of the “flu” didn’t go away. She Googled her symptoms and discovered that her mystery illness wasn’t an illness at all. She was one of the 20% of patients taking antidepressants who develop antidepressant discontinuation syndrome. The symptoms usually go away within a few weeks, but some people require more than a year. Her doctor had not warned her about this because he, too, was unaware of it. In medical school, we are taught mostly about the miracles of synthetic chemicals and less about the risks and side effects. This is partly because pharmaceutical companies have a significant disincentive to investigate and report the risks—especially the long-term risks—of their products.
Carol resumed her antidepressant and all her symptoms resolved. A few years later, she decided to risk those symptoms again. This time she was pleasantly surprised that it didn’t happen. However, within two months, she sank into a deep depression. “I guess I still need it,” she thought. She called her doctor for a refill and began to feel better again.

Everything was fine until a year later, when the drug stopped working. She couldn’t figure it out: She had a good job, wonderful husband, good kids, and good friends. “I have no reason to be depressed!” she protested. “It’s just a chemical imbalance,” her doctor replied. “You’ll just have to live with it.” He switched her to a newer-generation antidepressant, and she gradually started feeling better again.
While not universal, Carol’s experience is all too common. But it’s not as mysterious as it might seem. You see, neurons in the brain are designed to release neurotransmitters into a space called the synapse. The neurotransmitters migrate to nearby neurons and activate or block them from taking action, depending on what kind of neurotransmitter it is. Then the sending neurons suck the neurotransmitters back inside them through special channels. The neurotransmitters are then recycled and eventually released back into the synapse to do their thing again.
While the way antidepressants work has never truly been proven, researchers think they work by blocking the reuptake channel. With the neurotransmitters floating in the synapse longer, they can attach, release, and reattach to the receiving neuron. This works great, but it comes at a cost. There is an enzyme that lives in the synapse called monoamine oxidase, MAO for short. MAO breaks down neurotransmitters, making them inactive. Since they can’t enter the sending neuron through the reuptake channel, they also cannot be recycled. Consequently, over time, you end up with fewer neurotransmitters in your brain.
When you stop an antidepressant, not only do you have fewer neurotransmitters than you started with, but they are no longer kept in the synapse to keep you happy. As a result, you have a high risk of getting depressed again within 1-3 months. When it happens, you end up telling yourself you really do need that drug after all, even though the drug actually caused the problem.
Fortunately, Carol met a new coworker, Greg, who had successfully weaned off his antidepressant with the help of Prestige Wellness Institute. Greg benefitted from a two-pronged approach: he restored his neurotransmitter supply and identified and treated the original cause of his depression.
You see, neurons in the gut and brain make neurotransmitters from amino acids. When neurotransmitters are depleted, the body requires additional amino acids (beyond regular dietary proteins) to provide the raw materials for neurotransmitters. But simply taking a given amino acid won’t do the trick. Nor will protein powder. The body requires specific amino acids, and they need to be taken in a balanced mix. If one precursor amino acid is taken without or out of balance with others, it will block passage of the others from the bloodstream into the brain. This is why it is essential to take a balanced mixture of the correct amino acids, and to do so for at least six months.
At the same time, a sustained depression-free life requires treatment of the underlying cause of the problem. Trauma, loss, challenging relationships, and dysfunctional thought processes all benefit from a combination of therapy and functional medicine treatment. But when everything in a person’s life is beyond perfect except for the depression, medical causes need to be pursued. These include prescription drugs, deficiencies, toxicities, chronic infections, other chronic illnesses, unhealthy diet, gut dysfunction, old concussions, and much more. The benefit of identifying and treating these problems is that you can not only solve your depression or anxiety; you can also often solve other unexplained chronic health conditions.
If you have been unsuccessful in stopping your antidepressant, or are avoiding taking one in the first place because you would rather address the underlying problem, call Prestige Wellness Institute at (435) 210-0184 to schedule a consultation. Mental health problems are more widespread than at any time in history, and it’s not because genes have suddenly mutated and everyone has developed a chemical imbalance. There’s always a reason. Let’s find and fix it together.
|
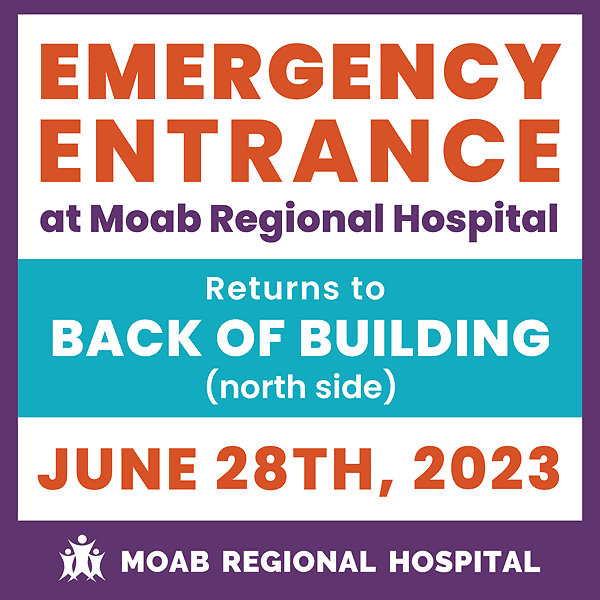
Moab Regional Hospital Opens New Emergency Department And Surgical Center
Moab Regional Hospital
|
On June 28, 2023, at 6:00 am, Moab Regional Hospital (MRH) will open its new and improved emergency department and state-of-the-art surgical center, part of a $30 million expansion that is scheduled for completion by summer 2024. MRH and its healthcare services are also expanding to cater to the evolving requirements of the community.
 Expanded clinic space for family medicine, specialists and mental health providers will open in August 2023. A retail pharmacy, and increased capacity in our diagnostic departments (e.g., lab and radiology, with a new CT scanner and MRI machines) are scheduled for completion summer 2024. Expanded clinic space for family medicine, specialists and mental health providers will open in August 2023. A retail pharmacy, and increased capacity in our diagnostic departments (e.g., lab and radiology, with a new CT scanner and MRI machines) are scheduled for completion summer 2024.
Moab Regional Hospital opened in 2011. A surge in tourism over the past decade increased the number of complicated traumas as well as the number of Urgent Care and Emergency Department patients, making additional Emergency Department space a high priority. The ER department has expanded from nine to 14 patient rooms, including a room specifically designed to manage complex psychiatric patients. As a certified Level IV Trauma Center, the new larger trauma bays will ensure the healthcare team has the space needed to care for critical patients.
Jennifer Sadoff, CEO of Moab Regional Hospital said, “It is exciting to see this project nearing the finish line. This expansion is funded by a USDA loan that refinanced our previous high-interest loan at one extremely low interest rate, but required that every dollar refinanced be matched with a dollar of new construction. At the end of this project, our community will have a hospital that is able to handle the needs of the foreseeable future, and has shell space designed in so future needs can be met without such a large effort. We are excited to see the positive impact this will have in the lives of our patients.”
The emergency department will feature:
1. Four new trauma rooms with state-of-the-art equipment that allows for better patient care.
2. Increasing the number of ER rooms from nine to 14 to reduce patient wait times.
3. A new isolation room where patients are kept separate from others while they receive medical care, typically for patients who have certain medical conditions or infections that affect the skin, lungs, airways, or intestines.
4. A quiet room where patients or their loved ones can speak with staff in a private and calm setting.
5. A new triage room where staff can conduct a preliminary assessment of the patient to determine the urgency of their need for treatment and the nature of treatment required.
6. A new, larger decontamination room that is equipped to help with the removal or neutralization of hazardous substances from people, equipment, and the environment before patients enter the hospital.
7. A larger and more comfortable waiting area
The surgical center will feature:
1. A central sterilization room where cleaning and sterilization of devices used in medical procedures take place.
2. New Operating Rooms with state-of-the-art “surgical booms” which are designed to centralize all surgical support equipment and utility services for operating room staff.
3. A biomedical room that provides a dedicated space for the repair, maintenance, and calibration of all biomedical equipment used in the hospital.
4. A new environmental services hallway which includes housekeeping and laundry services that are an integral part of keeping a hospital clean, orderly, and running smoothly.
To learn more and view videos about the expansion, visit www.mrhmoab.org/expansion.
Moab Regional Hospital is a 17-bed not-for-profit Critical Access Hospital and Level IV Trauma Center located in Moab, Utah, and is the leader in healthcare in southeastern Utah. Our mission is to put our patients first, deliver quality, cost-effective healthcare, and promote wellness to all we serve. From patient care to community wellness, Moab Regional Hospital serves as your portal to health.
Did you know that cancer survivorship begins the moment someone is diagnosed with cancer? June is National Cancer Survivor Month and an excellent time to raise awareness about the challenges of survivorship throughout all stages of the cancer journey. The challenges of a cancer diagnosis don't end when treatment ends.
How can I support a friend with cancer?
Ask permission. Before visiting, giving advice, and asking questions, ask if it is welcome. Be sure to make it clear that saying no is perfectly okay.
Make plans. Do not be afraid to make plans for the future. This gives your friend something to look forward to, which is especially important because cancer treatment can be long and tiring.
Be flexible. Make flexible plans that are easy to change if your friend needs to cancel or reschedule. The effects of cancer can be unpredictable.
Laugh together. Be humorous and fun when appropriate and when needed. A light conversation, a funny story, or a silly video or meme can make a friend's day.
Allow for sadness. Do not ignore uncomfortable topics or feelings if they come up. You may not be able to fix it, but you can provide comfort by just being with them. This may be called "holding space."
Check-in. Make time for a check-in phone call or text message. Your friend can respond to your outreach when they feel up to it.
Offer to help. Many people find asking for or accepting help hard, but your friend will likely appreciate the offer. Offer specific things you can help with, such as childcare, pet care, a ride to an appointment, or preparing a meal. If your friend declines the offer, do not take it personally.
Follow through. If you commit to helping them, it is important to follow through on your promise.
Treat them the same. Try not to let your friend's cancer get in the way of your friendship. As much as possible, treat them the same as you always have.
Talk about topics other than cancer. Ask about their interests, hobbies, and other topics not related to cancer. Come ready to talk to them about something unrelated to cancer. People going through treatment often need a break from talking about the disease.
Read their blog, web page, or group emails. Some people living with cancer choose a main avenue of communication to keep their support network updated. This can be writing a blog or social media page about their detailed experience that they can share with friends and family. Or a family member will post updates to a personal web page or send a group email or text. Stay current with these updates so your friend does not have to repeat experiences or information multiple times. These updates are also a great way to start a conversation and show that you care about what they are experiencing.
cancer.net supporting a friend who has cancer
|
|
|
|
|
|
|
|
|
© 2002-2026 Moab Happenings. All rights
reserved.
Reproduction of information contained in this site is
expressly prohibited.
|
|