|
|
HEALTHY HAPPENINGS - August 2021
|
Just Breathe
By Star Kolb |
You will do it 60-100 times during the course of an average article and you won’t even realize you are doing it.
It is an automatic process that exchanges gas and is essential to your life. It is BREATHING!
How many times in your life have you been aware of your breath? Maybe you have had your breath “taken away” by an amazing moment.
We will now ADD to our breath, we will add awareness and bring greater vitality to our mind and body.
When you inhale (breathe in), air enters your lungs and oxygen from the air moves from your lungs to your blood. At the same time, carbon dioxide, a waste gas, moves from your blood to the lungs and is exhaled (breathe out).
Seems easy enough?
It is amazing how many of us shallow breathe, hold our breath or breathe in and out through our mouths. This lessens the beautiful intrinsic design of our body. With practice we can increase the efficacy of our breathing process!
The breath works side-by-side with our physical structure, our body. When we have stress our natural tendency is to hold our breath or use stress-induced breathing, short and shallow. This increases or keeps the stress and tension in the mind and body.
Now imagine developing a relationship with your breath, one that you interact with as often as you like. This relationship with the breath becomes a conversation, a language unique to you. This conversation can detect stress, uneasiness, imbalance, once detected you can shift your breath, calm your nervous system and bring equanimity into your body and mind.
Let’s give it a try!
Come to a stable seated position(no slouching) or lie down.
Relax the muscles of your face and jaw, all the way down through the tips of your fingers and toes.
Hands to your belly. Steady breaths, feeling into the belly(try not to move the chest), in and out through the nose. 5-10 breaths.
Hands to chest/ribs. Steady and wide breaths into the chest/ribs(try not to move the belly), in and out through the nose. 5-10 deep breaths.
Now breathe into the belly and ribs/chest together, in and out through your nose.
Inhale-fill the lungs fully with a steady deep breath. Relax your body as you slowly exhale. 5-10 deep breaths.
This isn’t always comfortable at first, relax your breath in between as needed. With practice, bringing awareness to your breath will be welcomed, comfortable and relaxing.
Would you like to learn, practice, and experience more breathing techniques?
Join me, Star Kolb, for a FREE 4 Week Online Series where you gently learn more about your breath.
No experience needed, all you need is to have a comfortable spot to sit and to lie down.
Breath Series: Thursdays August 5, 12, 19, 26. 4-4:25pm. Register: www.starkolb.com/classes (www.Sundari-Designs.com)
|
USU Moab Launches Community Healthcare Certificate Program
by Loren Miller, University Marketing & Communications, USU |
Utah State University Moab has launched a new certificate program. Students can now earn the community healthcare worker certificate, which is awarded upon completion of the 18-module course. Graduates of the course are granted a certification from the Utah Department of Health Environment, Policy & Improved Clinic Care (EPICC) program.
The first cohort of the program already started and was be completed at the end of June. The program is designed to be completed in 9-12 weeks.
“The CHW cohort is a fantastic opportunity for students and certified graduates to be recognized and participate in a formal and intensive training to support their existing experiences assisting their communities,” said CHW program facilitator Maria Velasco Burgos. “Students also network and connect with different organizations that can help them build their projects depending on their population focus or interest. Facilitators have solid and individualized relationships with students to ensure they assist them in getting the most from the program.”
 |
| USU Moab students Kolby Williams and Gail Wakefield and other members of the first Community Healthcare Workers certificate cohort. |
The Community Health Worker Core Skills Certification provides training on the implementation of innovative prevention strategies outside of the clinical setting and interventions that will reach whole populations and not only those with access to the traditional healthcare system.
“Rural communities have a lot of public health barriers and are affected by many disparities’ issues,” Velasco Burgos said. “This program is a great way to help the Moab community to address its challenging health problems. Students are part of different local organizations and are being able to be work with specific populations already.”
The program is self-paced, with class members meeting twice a week to receive help with coursework and to walk through the modules. The students complete the program with an apprentice style practicum in the field, performing community health work in various locations in Moab. Through the program, participants will complete core competency training in advocacy, outreach, capacity building, individual and community assessment, care coordination and system navigation, interpersonal skills and relationship building, popular education and facilitation, professional conduct, communication, and knowledge.
The certification program was created to address a growing need for community health workers in the rural parts of the state of Utah. These workers would fill gaps resulting from primary and mental health care having limited availability and unable to meet the demand in a geographically distanced and economically evolving rural areas, such as Moab. This program is financed through two grants, the Governor’s Office of Economic Development Learn & Work grant and the Utah State Board of Education Perkins V “Special Projects Grant.”
Students interested in the program should reach out to Maria Velasco Burgos (maria.velascoburgos@usu.edu) in order to receive an application. Applications are sent to the Utah Department of Health EPICC Program and the Utah Community Health Worker Association (UCA). UCA prioritizes applications based on level of community involvement, years working as a community health worker, cultural abilities to reach underserved populations, motivation and purpose, and other factors.
Those selected for the cohort are accepted to USU Moab and will receive the training free of charge. Those not selected will be eligible to be selected in future cohorts. Applications for the next cohort, which will begin in July, are currently being accepted.
|
Need a Boost?
By Ray Andrew, MD |
|
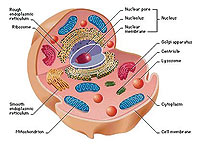
Ever feel like you could use a boost? Cells of your body get their energy from the metabolism (think of it as combustion) of fat and carbohydrates in the presence of oxygen. This process occurs in tiny power plants called mitochondria. Each cell can have hundreds or thousands of mitochondria, depending on its energy needs.
Most of us have no problem supplying our mitochondria the fat and carbohydrates they need, but we often have more difficulty getting them the vitamins and minerals they need to convert those calories into usable energy. One reason for this is nutrient-deficient soil from maximum-yield farming techniques and pesticide/herbicide use. Another is (usually unrecognized) damage to the intestinal lining due to stress, glyphosate (aka Round Up), antibiotics, steroids, alcohol, brain concussion, prescription drugs, and other insults. Some prescription drugs damage the gut lining inadvertently while others damage it intentionally—with grave long-term consequences—in order to increase the absorption of the drug into the bloodstream.
 But mitochondria need more than just a healthy, organic, non-GMO diet, or even supplementation with vitamins and minerals. By way of analogy, a truckload of cement and bricks unloaded onto your driveway does not magically make a fence in your backyard. Someone with the correct tools and instructions has to transport those raw materials into the backyard and organize them into a fence in the precise location you want it, and at the desired height. Similarly, mitochondria need instructions (signals) from hormones like testosterone, cortisol, thyroid hormone, and DHEA to convert calories into ATP, the energy each cell needs for all of its operations. But mitochondria need more than just a healthy, organic, non-GMO diet, or even supplementation with vitamins and minerals. By way of analogy, a truckload of cement and bricks unloaded onto your driveway does not magically make a fence in your backyard. Someone with the correct tools and instructions has to transport those raw materials into the backyard and organize them into a fence in the precise location you want it, and at the desired height. Similarly, mitochondria need instructions (signals) from hormones like testosterone, cortisol, thyroid hormone, and DHEA to convert calories into ATP, the energy each cell needs for all of its operations.
Supposing you have an adequate supply of both nutrients and hormones, you may still find yourself feeling like you’re out of gas. This can be due to increased demand for those nutrients. This can happen when you are under stress; sick; after surgery; or after a good ride, workout, or hike.
Whether your problem is inadequate supply or increased demand, IV nutrition can help. In fact, some people choose to take advantage of IV therapy before they have surgery, or go on a big adventure, so they can have that added boost they need. Others come in for IV nutrition and/or oxidative therapy (using medical ozone) when they are under the weather with a respiratory or gastrointestinal illness. Rehydration therapy, which is different from IV nutrition, can be a very inexpensive alternative to an E.R. visit when you’ve been out in the Moab heat a little longer than your body could handle.
 Even under the best of circumstances, your body’s absorption of nutrients from your food is far less than what you took in. You can only absorb so much at once. The advantage of IV nutrition is that, no matter what is going on in your gut, absorption of IV nutrients into your bloodstream is 100%. Even under the best of circumstances, your body’s absorption of nutrients from your food is far less than what you took in. You can only absorb so much at once. The advantage of IV nutrition is that, no matter what is going on in your gut, absorption of IV nutrients into your bloodstream is 100%.
But supply, signaling, and demand are not the full mitochondrial story. Yet another critical factor is interference. Heavy metals such as mercury, lead, arsenic, aluminum, and cadmium block the actions of enzymes that are necessary for energy production in this powerhouse of the cell called the mitochondrion. Everyone has heavy metals in their organs and fat cells, some more than others. And they started accumulating even before you were born, because you get them from your mother. IV chelation is the process we use to remove heavy metals from the organs and tissues of your body.

Finally, increasing numbers of patients with cancer are utilizing supportive therapy with high-dose IV vitamin C (HDIVC). Structurally, vitamin C looks so similar to glucose that high doses in the bloodstream actually trick glucometers into reading high sugar levels. More importantly, because cancers feed mostly on sugar, they eagerly welcome vitamin C inside (thinking it is sugar), where this Trojan horse causes so much oxidation that the cells can’t survive. Whereas this therapy alone is never recommended for the treatment of cancer, HDIVC has been shown in studies to enhance the effectiveness of whatever other treatments are employed.
These are some of the health-enhancing IV therapies offered every day at Prestige Wellness Institute. We do not skimp on the nutrients your mitochondria crave, as is often the case with franchise IV clinics. And we always have a medical provider/supervisor on site. Whether it’s our beefed-up Myers Metabolic Cocktail or one of our many other personalized IV therapies, now is a good time for a boost! Call (435)259-4008 to make an appointment for whichever IV therapy you need.
|
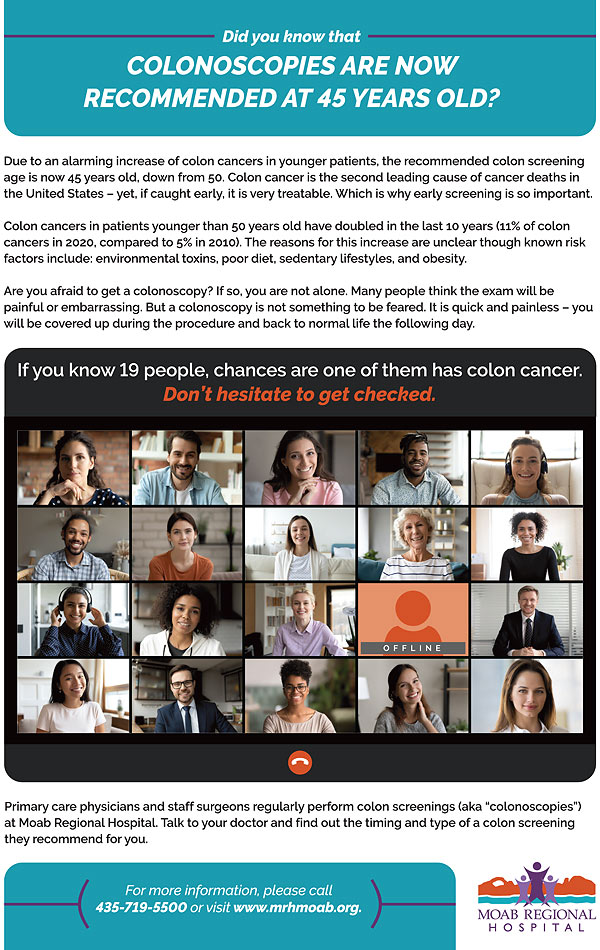
| “45 is the new 50” for Colorectal Cancer Screening |
Colorectal cancer is the second leading cause of cancer deaths in the United States, with almost 52,000 deaths in 2019. In general, however, it is a slow  growing cancer that is treatable if caught early enough, and in fact it can actually be prevented. That’s where screening comes in. In the past, screening was advised starting at age 50, but prompted by an alarming increase in colorectal cancers in younger patients, an independent expert panel has recommended that individuals at average risk for the disease start the screening process at age 45. This change in guidelines advocated by the U.S. Preventative Services Task Force (USPSTF) now aligns with that of the American Cancer Society, which made the recommendation for a lower screening age of 45 in 2018. The task force recommendation means that insurers will be required to cover preventative procedures such as stool tests and colonoscopies that can detect colorectal cancer at an early stage. growing cancer that is treatable if caught early enough, and in fact it can actually be prevented. That’s where screening comes in. In the past, screening was advised starting at age 50, but prompted by an alarming increase in colorectal cancers in younger patients, an independent expert panel has recommended that individuals at average risk for the disease start the screening process at age 45. This change in guidelines advocated by the U.S. Preventative Services Task Force (USPSTF) now aligns with that of the American Cancer Society, which made the recommendation for a lower screening age of 45 in 2018. The task force recommendation means that insurers will be required to cover preventative procedures such as stool tests and colonoscopies that can detect colorectal cancer at an early stage.
In 2020 11% of colon cancers and 15% of rectal cancers occurred in patients younger than 50 years, compared to 5% and 9%, respectively, in 2010. Colorectal cancer is even being seen in increased frequency in patients in their 20s and 30s and by 2030 is expected to be the leading cause of death from malignancy for people in their twenties through forties.
The reasons for this increase are unclear though there are several known risks factors: environmental toxins, poor diet, sedentary lifestyles, and obesity.
In addition, another major study has found that continuing colorectal cancer screening past the age of 75 is felt to be beneficial for some people, whereas previously it was generally advised to stop screening in these patients.
Colonoscopy is considered to be the “Gold Standard” of colorectal cancer screening. This is because the test physically looks at the lining of the intestine, and also because pre-cancerous polyps can be removed before they ever get the chance to turn into malignant growths. There aren’t many cancers where we can intervene in such a way. Another benefit is that with a normal exam, the next one will not be necessary for ten years, depending on one’s personal and family history.
Are you afraid to get a colonoscopy? If so, you are not alone. Many people think the exam will be painful or embarrassing. In fact, in spite of the preventative benefits of colorectal cancer screening, only around 70% of eligible individuals in the United States undergo screening. But colonoscopy is not something to be feared. It is quick and painless, you will be covered up during the procedure, and you can be back to normal life the following day.
In addition, there are other methods of screening available, including stool tests which need to be done every one to three years. These are all effective screening methods and some are quite inexpensive. If you are unsure which test is best for you, discuss it with your healthcare provider.
Our current guidelines for screening are:
Average risk, start at age 45. People in good health with a life expectancy more than 10 years should continue regular screening through the age of 75.
For people ages 76 through 85, the decision to be screened should be based on a person’s preferences, overall life expectancy, overall health, and prior screening history.
People at higher risk may need earlier and more frequent screening. This includes people with a personal or a strong family history of colorectal cancer or certain kinds of polyps; a history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease); hereditary colorectal cancer syndromes; or a history of radiation to the abdomen or pelvis.
With all of the alternatives available, there is no reason not to get screened for colorectal cancer. No test is perfect, but there is a test that is right for you. So whatever one you choose, just get screened. It is one of the best decisions you can make for your future health.
|
|
|
|
|
|
|
|
© 2002-2024 Moab Happenings. All rights
reserved.
Reproduction of information contained in this site is
expressly prohibited.
|
|